Home » Health News »
A global view on fatty liver and diabetes helps to fight other non-communicable diseases and COVID-19
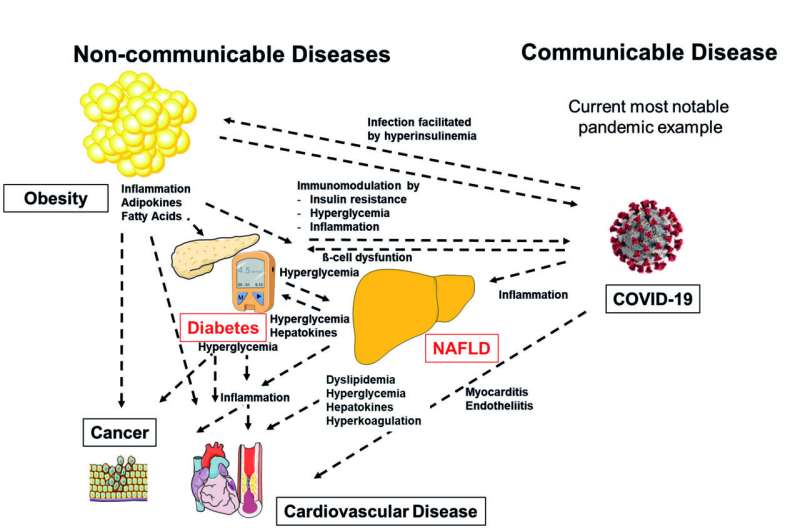
Non-alcoholic fatty liver disease (NAFLD) has become an epidemic, similar to the non-communicable diseases cancer, obesity, cardiovascular disease and diabetes. In a review article in The Lancet Diabetes & Endocrinology, Norbert Stefan and Kenneth Cusi first highlight the extent to which NAFLD and diabetes jointly occur worldwide. Then they address the major mechanisms that are involved in the pathogenesis of NAFLD and type 2 diabetes and discuss whether these mechanisms place NAFLD in an important position to better prevent and treat non-communicable diseases and the communicable disease COVID-19. Finally, using a holistic approach, integrating knowledge from early childhood development to older age, they propose solutions how this knowledge can be used for personalized prevention and treatment of NAFLD in the future.
Worldwide more than 25% of adults and 3-10% of children have NAFLD. These numbers increase to about 60% and 40% in adults and children with obesity and/or diabetes. These numbers are alarming, because NAFLD, and more so non-alcoholic steatohepatitis (NASH) and NAFLD-associated hepatic fibrosis, increase the risk of advanced liver diseases (e.g. hepatic cirrhosis, hepatic cancer) and cardiometabolic diseases (e.g. cardiovascular disease, type 2 diabetes).
Professor Kenneth Cusi from the University of Florida (USA) says that “because the highest prevalence of NASH and hepatic fibrosis is observed in patients with type 2 diabetes, the disease which epidemically increased during the past decades, focusing on the interplay of NAFLD with type 2 diabetes may help to better understand the major mechanisms that propel the worldwide increase of NAFLD.” By doing just that, the authors identify increased energy-dense food and fructose consumption, as well as genetically-determined visceral fatness and impaired capacity of fat deposition in the lower part of the body as important drivers of NAFLD and type 2 diabetes. The interplay of fatty liver and diabetes, involving subclinical inflammation, insulin resistance, increased glucose levels, dysregulated liver-derived proteins (hepatokines), dyslipidemia and hypercoagulation of the blood, amplifies the impact both diseases on each other, as well as of an unhealthy lifestyle and genetic risk on the development of other non-communicable diseases, such as cancer and cardiovascular disease. Importantly, the same mechanisms (subclinical inflammation, high glucose levels and insulin resistance) also increase the risk of a severe course of COVID-19.
Professor Norbert Stefan from the University of Tübingen, the Institute for Diabetes Research and Metabolic Diseases (IDM) of the Helmholtz Zentrum München (Germany), a partner of the German Center for Diabetes Research (DZD), adds that “metabolic pathways are key in understanding why NAFLD develops and how it impacts on other diseases. Therefore, it is now time to use a holistic approach to study the pathogenesis of NAFLD.” This proceeding involves the integration of knowledge about non-modifiable risk factors, such as genetically-determined fatty liver and unhealthy storage of fat and aging-associated redistribution of fat and decrease in muscle mass. Furthermore, modifiable risk factors, such as malnutrition in early and later stages of life, and metabolic risks, such as high glucose and insulin levels, need to be early on identified and treated.
Source: Read Full Article



