Home » Health News »
New study finds high-touch surfaces in care facilities are frequently contaminated with potentially infectious material
Findings from a study published today in the American Journal of Infection Control (AJIC) provide new insights that could help long-term care (LTC) facilities assess the cleanliness of high-touch surfaces, and thereby enhance infection prevention and control measures designed to prevent serious diarrheal diseases and deaths among their residents. The study evaluated the utility of specific hygienic monitoring tools for assessing levels of microbial contamination on high-touch surfaces in 11 LTC facilities in South Carolina.
“Our study is among only four conducted to date evaluating environmental hygiene in LTC facilities,” said Jennifer Cannon, Ph.D., CDC Foundation field employee working with the Centers for Disease Control and Prevention (CDC), and the paper’s lead author. “Increasingly, hospitals are performing routine audits of high-touch surface cleanliness, helping to reduce morbidity and mortality among residents. Our results suggest similar auditing programs would benefit LTC facilities when included as part of their infection prevention programs.”
Diarrheal illnesses caused by norovirus and C. difficile infections (CDI) are among the most frequent healthcare-associated infections in LTC facilities; in the United States, approximately 60% of norovirus outbreaks and more than 50% of all healthcare-associated CDI occur in LTC facilities. Both pathogens can be transmitted by environmental surfaces contaminated with fecal matter. While environmental monitoring using surface hygiene indicators is a valuable tool to help prevent the spread of infection, there are no standard technologies or methodologies, and many monitoring tools are too expensive to be used routinely.
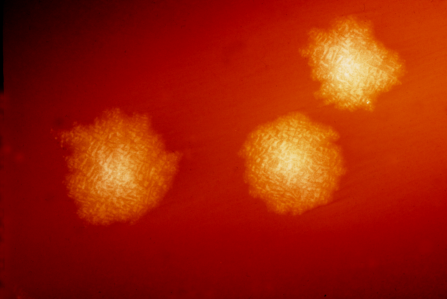
For their study, Dr. Cannon and her colleagues used three tools to evaluate the cleanliness of a minimum of 30 surfaces in each of 11 LTC facilities in South Carolina: adenosine triphosphate (ATP), a bioluminescent chemical reaction that indicates the presence of organic material; norovirus; and crAssphage, a recently discovered DNA bacteriophage that indicates past or present fecal contamination. Their study was the first to utilize crAssphage as a fecal contamination indicator in the LTC setting.
Ninety percent of the high-touch surfaces the researchers tested (n=337) were positive for crAssphage or had organic material levels that resulted in failing ATP cleanliness scores.
- crAssphage was detected on 311 (92.3%) surfaces, often at high levels (median concentration 3.5 log genomic copies).
- Nearly all surfaces 324 (98%) had high levels of ATP, resulting in a “failing” score using threshold values suggested by the ATP kit manufacturer.
- All 337 surfaces tested negative for norovirus. The researchers suggest that this finding is consistent with previous studies suggesting noroviruses are rarely detected in the absence of a current or recent outbreak.
Aggregating data from all 11 facilities, Dr. Cannon and colleagues combined the ATP and crAssphage tools to identify the types of surfaces and locations most likely to be contaminated by organic or fecal material:
- Handrails and equipment controls were four times more likely to have high levels of crAssphage than other surfaces and locations (odds ratio [OR] 4.1, CI 2.0-8.5, p < 0.001 for handrails; OR 3.6, CI 1.1-12.8, p < 0.05 for equipment controls).
- Patient bed handrails as well as tables and chairs in patient lounges had high levels of both ATP and crAssphage.
- Locations in LTC facilities more likely to have high levels of crAssphage were patient beds (OR 3.9, CI 1.4-12.3, p < 0.05) and hallways (OR 2.6, CI 1.3-5.0, p < 0.01).
- Surfaces touched by patients and visitors were twice as likely to have high levels of ATP compared to those touched primarily by nursing and janitorial staff or by patients alone.
Source: Read Full Article

