Home » Health News »
Discovering what makes Shiga toxin so damaging
E. coli food poisoning is one of the worst food poisonings, causing bloody diarrhea and kidney damage. But all the carnage might be just an unintended side effect, researchers from UConn Health report in the 27 November issue of Science Immunology. Their findings might lead to more effective treatments for this potentially deadly disease.
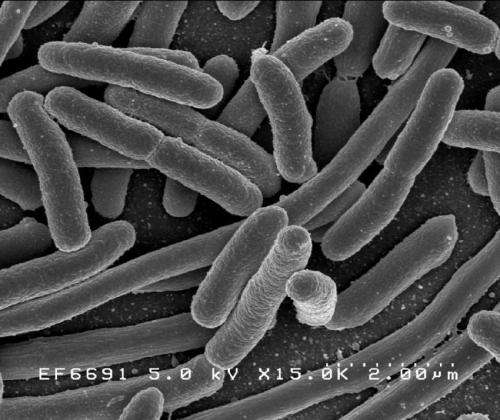
Escherichia coli are a diverse group of bacteria that often live in animal guts. Many types of E. coli never make us sick; other varieties can cause traveler’s diarrhea. But swallowing even a few cells of the type of E. coli that makes Shiga toxin can make us very, very ill. Shiga toxin damages blood vessels in the intestines, causing bloody diarrhea. If Shiga toxin gets into the bloodstream it can cause kidney failure.
“This is especially common in children; about 15% of kids with Shiga toxin-producing E. coli infections get kidney disease, and some can suffer long term kidney damage,” says UConn Health immunologist Sivapriya Vanaja.
A group of Shiga toxin-producing E. coli called enterohemorrhagic E. coli, or EHEC, are especially common in the United States. When you hear that a batch of romaine lettuce is being recalled because of a dangerous outbreak of food poisoning, it’s almost certainly due to EHEC.
EHEC normally live in cattle without making them sick. It used to be relatively common to have EHEC outbreaks coming from unhygienically prepared ground meat, but stringent regulations on slaughterhouses have made this less common. Now it’s more likely for EHEC to appear on vegetables grown in fields adjacent to cattle or manure runoff.
But no matter where it comes from, once EHEC bacteria get inside a human, the infection is hard to treat. Antibiotics tend to make it worse—when the bacteria feel themselves dying, they make more Shiga toxin. And EHEC are very good at inhibiting the part of the immune system that normally responds early to this kind of infection, allowing them to grow unchecked in the human gut.
In a study led by Morena Havira, a postdoctoral fellow in Vanaja’s lab, the team wanted to know how EHEC suppresses the immune system. The body normally responds to early stages of E. coli infections by activating an enzyme that kicks off an alarm inside cells. The cell bursts open to release a cloud of warning molecules that call other parts of the immune system to come and fight the bacteria.
But EHEC squashes that early response. To figure out how it does that, Vanaja and her colleagues decided to see which individual gene in EHEC was responsible. They took many different varieties of EHEC from a bacterial mutant library, and infected immune cells with them.
The team found that cells infected with EHEC that was missing the gene for Shiga toxin mustered a higher immune response compared to normal EHEC.
“It was surprising. Shiga toxin is very well-studied for its toxic activity; it wasn’t known that it had another function,” Dr. Vanaja says. So Shiga toxin’s stealthy suppression of the immune system may have a link to all the bloody drama that ensues. Spurred on by this exciting observation, they conducted a series of detailed molecular studies, which revealed that Shiga toxin blocks a protein from bursting open the infected cell and alerting the body of infection.
Source: Read Full Article



