Home » Health News »
In situ vascular tissue engineering: Methods, models, and mechanisms
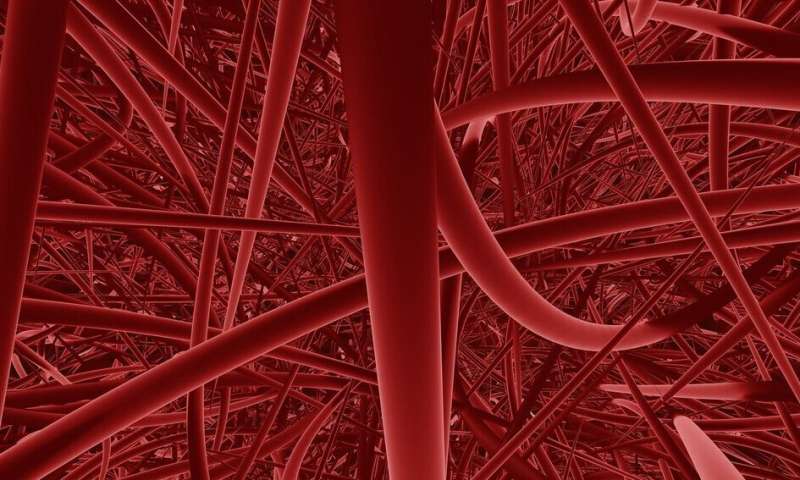
Biodegradable plastic scaffold implants can help replace damaged vascular tissue in the body. The implant is placed in the body and prompts the body to replace the plastic with blood vessel cells. In addition, the scaffolds can also control immune and cell growing responses. Suzanne Koch designed methods and models to improve our understanding of how tissue engineered vascular grafts based on biodegradable materials can be used in clinical practice.
A biodegradable plastic scaffold that upon implantation prompts the body to replace the plastic with a living own-grown blood vessel. That is the basic idea behind material-driven in situ tissue engineered vascular grafts. Besides replacing tissue functionality upon implantation, these scaffolds should control the host’s immune and tissue producing cell responses to grow new functional vascular tissue, while slowly resorbing the scaffold.
This approach might be a solution for the shortage of blood vessels needed to treat cardiovascular patients who require replacement or bypass of a malfunctioning vessel. Or for kidney patients who may require a vascular access for dialysis treatment.
For her Ph.D. research, Suzanne Koch investigated, designed, and applied methods, models, and mechanisms to gain a better understanding on the use of safe and reliable in situ vascular tissue engineering approaches using cell-free resorbable materials.
Surveying the literature
In her thesis, Koch showed that the addition of pro-regenerative signaling molecule interleukin-4 (IL-4) led to early immune response to implants, which were implanted as blood vessel replacement in laboratory rats. After 3 months of implantation, the tissue build-up also improved.
Although the laboratory rat is regularly used for the preclinical assessment of in situ tissue engineered vascular grafts (TEVGs), preclinical standards for the use of the animal model, study design, or read-out parameters have not been defined or consented on. This hampers inter- and intra-study comparisons, and thus a fast transition to clinical use.
To provide input for formulating such a standard, we systematically evaluated all published preclinical studies assessing available cell-free off-the-shelf resorbable synthetic in situ TEVGs across a total 182 publications. Analysis on graft patency (if the blood vessels stay ‘open’) showed that for species, age, sex, implantation site, and follow-up time model-specific variations exist. The large overview in our systematic review provides the first leads for defining a standard, and identified current bottlenecks in study design and reporting of animal experiments that are necessary to increase translational value.
Influence of high sugar levels
In the second part of her thesis, Koch employed various advanced in vitro platforms to assess fundamental processes in the in situ vascular TE process.
She studied the influence of high sugar levels (common in diseases like diabetes) on the macrophage and tissue producing cell responses to degradable materials. She also investigated the effects of hemodynamic loading on the regenerative capacity of small blood vessels grown in an advanced custom-developed bioreactor.
And finally, Koch used cells from human vascular organoids (made from reprogrammed skin cells) to culture mini-blood vessels in the lab. In the future, this technique can be used to establish patient-specific laboratory models for (cardio)vascular diseases and personalized drug treatment research, by harvesting the patient’s own cells in a non-invasive way.
Impact
The results of Koch’s research show that the impact of patient-specific factors on the immuno-regenerative response cannot be ignored, and that it is important to take these factors into account in future research. Herein lies a potential role for in vitro studies employing advanced bioreactors and cell sources to provide a better understanding of the underlying mechanisms of material-driven vascular tissue regeneration, with the aim to contribute to a safe clinical application of in situ TEVGs.
Source: Read Full Article


