Home » Health News »
Aching joints make older adults reach for many forms of pain relief—but health risks could follow
Popping a pill may bring short-term relief for arthritis-related joint pain, but many older adults may not realize that what they swallow could raise their risk of other health problems, or that other non-drug options could help them, a new poll suggests.
Even if they’re managing the pain on their own, people over 50 should talk to their health care providers about what they’re taking, and get advice about potential medication risks and non-medication options that could also relieve their aches and improve their movement, the poll’s authors say.
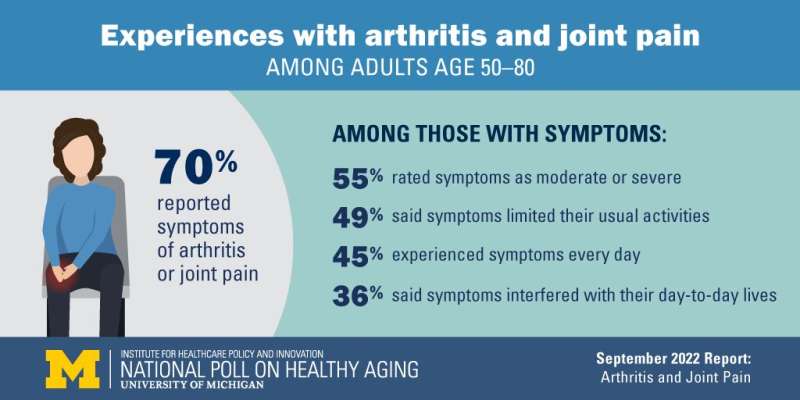
The new results from the University of Michigan National Poll on Healthy Aging show that 70% of people over 50 experience joint pain at least occasionally, and 60% have been told they have some form of arthritis. Nearly half of those with arthritis symptoms said they have pain every day (45%). About half of those with joint pain say the pain limits their usual activities at least somewhat (49%), while a over a third (36%) say it interferes with their day-to-day life.
The poll is based at the U-M Institute for Healthcare Policy and Innovation and supported by AARP and Michigan Medicine, U-M’s academic medical center.
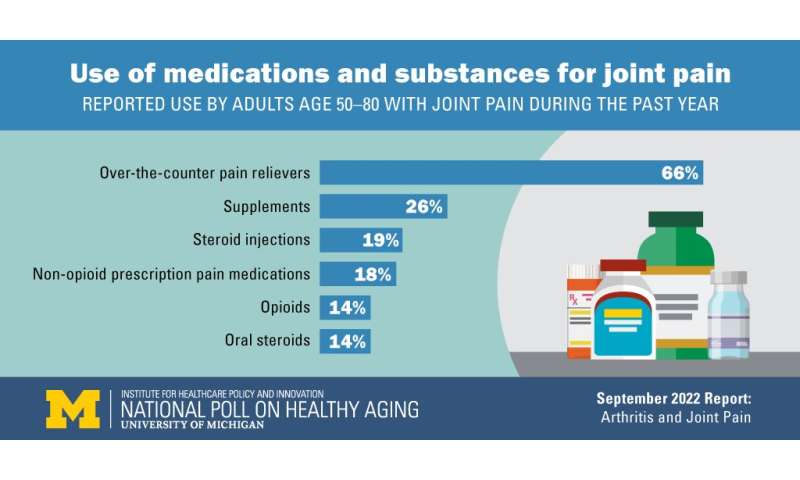
The vast majority (80%) of those with joint pain said they had at least some confidence they could manage it on their own. The poll shows many do so with non-prescription remedies: 66% of those with joint pain take over-the-counter pain relievers such as aspirin, acetaminophen, ibuprofen or naproxen. More than a quarter (26%) say they take supplements, (such as glucosamine or chondroitin) while 11% have turned to cannabidiol (CBD, derived from marijuana) and 9% use marijuana.
But a sizable minority have turned to prescription-based treatments including prescription-only non-opioid pain relievers (18%), steroid joint injections (19%), oral steroids (14%), opioids (14%) and disease-modifying anti-rheumatic drugs (4%).
“There are sizable risks associated with many of these treatment options, especially when taken long-term or in combination with other drugs. Yet 60% of those taking two or more substances for their joint pain said their health care provider hadn’t talked with them about risks, or they couldn’t recall if they had. And 26% of those taking oral steroids hadn’t talked with a provider about the special risks these drugs bring,” says Beth Wallace, M.D., M.S.
Wallace is a rheumatologist and researcher at the VA Ann Arbor Healthcare system, the VA Center for Clinical Management Research and Michigan Medicine who has studied medication interactions in arthritis. She adds, “This suggests a pressing need for providers to talk with their patients about how to manage their joint pain, and what interactions and long-term risks might arise if they use medications to do so.”
She notes that the American College of Rheumatology’s latest guidelines for treating osteoarthritis—the most common form of arthritis—and the more-rare rheumatoid arthritis both emphasize an evidence-based approach to joint pain for clinicians and patients to follow.
The guidelines seek to reduce the risk that medications will affect patients’ stomach, liver, blood pressure, blood sugar, mood or sleep. These risks rise with long-term use and in people who take multiple medications or certain supplements, as well as those who drink alcohol regularly.
For osteoarthritis, which is sometimes called “wear and tear” or degenerative arthritis, the guideline emphasizes weight loss; exercise; self-management programs with arthritis educators; tai chi; yoga; braces, splints and kinesiotaping; acupuncture or acupressure; cognitive behavioral therapy and applying heat, cold or topical pain relievers on aching joints.
The poll shows 64% of those with joint pain do use exercise, and 24% have had physical therapy, which is also in the osteoarthritis guideline. But far fewer used non-drug options such as braces.
For medications, the osteoarthritis guideline focuses on short-term use of over-the-counter pain medications, in as low a dose as possible, as well as steroid joint injections in appropriate patients. But it recommends against most supplements, and against opioids and other prescription drugs because of a lack of evidence or evidence of risk.
The poll shows that certain groups of older adults appear to be more likely to experience worse joint pain, especially at a level that interferes with their lives or activities, says poll director Preeti Malani, M.D., a Michigan Medicine physician with training in infectious diseases and geriatrics.
“Those who say their overall health is fair or poor were twice as likely to say they have moderate or severe joint pain as those in better health. The difference was nearly as great between those who say their mental health is fair or poor than those who reported better mental health,” she says. “And older adults with fair or poor physical or mental health were much more likely to agree with the statement that there’s nothing that someone with joint pain can do to ease their symptoms, which we now know to be untrue. Health providers need to raise the topic of joint pain with their older patients, and help them make a plan for care that might work for them.”
Source: Read Full Article



