Home » Health News »
Carcinogen-exposed cells provide clues in fighting treatment-resistant cancers
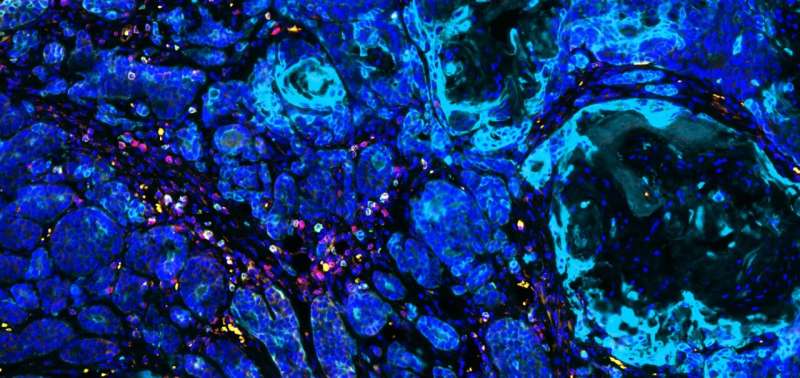
Researchers from Massachusetts General Hospital (MGH) have discovered a biological mechanism that transforms cells exposed to carcinogens from environmental factors like smoking and ultraviolet light into immunogenic cells that can be harnessed therapeutically to fight treatment-resistant cancers. As reported in Science Advances, that mechanism involves spurring the release of small proteins known as chemokines which, in turn, recruit antitumor immune cells (CD8+ T cells) to the tumor site to block metastasis, potentially enhancing the effectiveness of a new generation of immunotherapies.
“Immunotherapeutics have shown tremendous promise in recent years, but the fact is their response rate for many types of cancers is very low,” says senior author Shadmehr (Shawn) Demehri, MD, Ph.D., an investigator in the Center for Cancer Immunology and the Cutaneous Biology Research Center at MGH. “We showed how cells exposed to certain carcinogens become immunogenic, that is, become targets for the immune attack, and how that exposure might be exploited to treat such major forms of cancer as breast and other epithelial cancers.”
CD8+ T cells are known to effectively attack the cells exposed to environmental carcinogens. But in the past, science has focused mainly on the mutations caused by these exposures in a patient’s heritable DNA as the reason for the immune attack. In their laboratory work with mice, the MGH team demonstrated for the first time another consequence of carcinogen exposure that can have significant immunologic implications, namely, the nongenetic alteration of cells through such harmful environmental factors as smoking, ultraviolet light and pollution.
“This finding is particularly important because it could open the door to therapeutic interventions that aren’t practical with a DNA approach, since no clinician wants to introduce even more genetic mutations into cancer cells just to make them more immunogenic,” explains Demehri. “We learned if there was another immunogenic element associated with carcinogen exposure independent of or even complementary to the presence of the mutation, then you could deliver that factor into a ‘cold’ tumor to make it ‘hot,’ meaning it would become immunogenic and responsive to immunotherapies.”
That factor is a chemokine known as CCL21, which MGH researchers found to be expressed in breast cancer cells in mice that were exposed to DMBA, a carcinogen similar to that found in cigarette smoke. “Through its signaling, CCL21 recruits CD8+ T cells which infiltrate the tumor, as previous work has shown, and are associated with a significant reduction in relative risk of distant metastasis,” says lead author Kaiwen Li, MD, an investigator in MGH’s Center for Cancer Immunology, MGH’s Cutaneous Biology Research Center and the Department of Urology at Sun Yat-sen Memorial Hospital at China’s Sun Yat-sen University. “Not only does CCL21 induce an antitumor immune response to prevent metastasis, but it overcomes other immune cells known as Tregs (immunosuppressive regulatory T cells) present in tumors from inhibiting the work of the CD8+ T cells.”
As an example of how this unique mechanism could be used therapeutically, the MGH team reported that an injection of CCL21 into the tumor might be able to transform cold breast cancers into hot tumors responsive to current immunotherapies.
Source: Read Full Article



