Home » Health News »
COVID-19 presents a higher risk of blood clots than vaccination
The coronavirus disease (COVID-19), which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), continues to wreak havoc across the globe. To date, more than 221 million people have been infected with SARS-CoV-2 and over 4.5 million have died as a result of this disease.
The most extensive study on post-vaccine side effects has recently been published in the British Medical Journal (BMJ). To this end, this study found that people were at a slightly higher than normal risk of blood clots after receiving a ChAdOx1 nCoV-19 (Oxford-AstraZeneca) and BNT162b2 mRNA (Pfizer-BioNTech) vaccines. For short time intervals following the first dose, there is a heightened risk of thrombocytopenia and thromboembolism leading to hospitalization or death.
However, the team noted that the risks are considerably higher if these same individuals were to get COVID-19 as compared to after they received either vaccine.
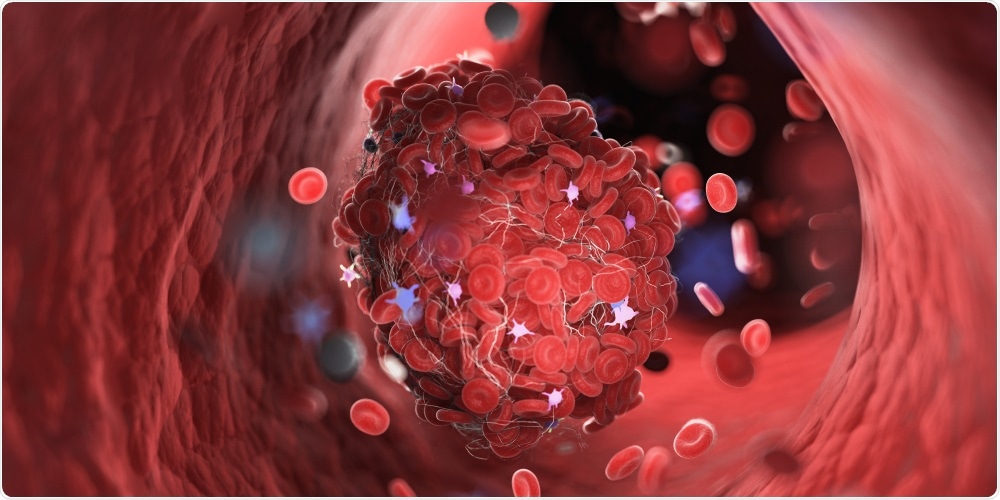 Study: Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. Image Credit: SciePro / Shutterstock.com
Study: Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. Image Credit: SciePro / Shutterstock.com
Increased risk of blood clots
COVID-19 vaccines have been tested in randomized clinical trials to determine their efficacy and safety. These trials are insufficiently driven to detect rate adverse events.
Amid the vaccination campaigns, when a vaccine has a severe adverse profile, even if the risk is rare, a risk-benefit evaluation could cause the vaccine's withdrawal or restrictions on its use. It is therefore crucial to ensure that the risks of vaccination are balanced against the risk of COVID-19 in terms of their ability to cause adverse events and death.
Since December 2020, vaccination efforts have commenced in many countries worldwide. Recently, thromboembolic events after receiving the Oxford-AstraZeneca have been reported in Denmark, Germany, Norway, Austria, and the United Kingdom.
These events prompted many countries to limit the use of the vaccine. The United States has also reported blood clots tied to the Ad26.COV2-S (recombinant) Janssen vaccine, which temporarily halted the roll-out of this vaccine until further investigation indicated that the risk was extremely rare to those receiving this vaccine.
Vaccine short term risks
In the current study, researchers assessed the link between COVID-19 vaccines and the risk of thrombocytopenia and thromboembolic events in England among adults.
The current study is the largest of its kind, as it included over 29 million vaccinated people following their first doses between December 1, 2020, and April 24, 2021. The participants were above 16 years old who had received their first doses of either the Oxford-AstraZeneca or Pfizer-BioNTech vaccines. The researchers compared rates of adverse events after vaccination with the same events after being diagnosed with COVID-19.
To arrive at the study findings, the team utilized the National Immunization Management System register of COVID-19 vaccination to determine vaccine exposure. This includes the vaccine type, date, and doses for all people vaccinated in England. The team also linked individual-level data to national data for mortality, hospital admissions, and COVID-19 infection.
Study findings
In the eight to 28 days after patients had received the first dose of the Oxford-AstraZeneca vaccine, an increased risk of rare blood clotting events and low platelet counts were reported. In the same period after the first dose of the Pfizer-BioNTech vaccine, an increased risk of blood clots and strokes due to the restricted blood flow to the brain have also been reported.
However, the researchers noted that these adverse effects were much higher following SARS-CoV-2 infection.
The study also estimated that 107 people for every 10 million people exposed to the Oxford-AstraZeneca vaccine might develop thrombocytopenia, 66 for venous thromboembolism, and seven for cerebral venous sinus thrombosis (CVST). Meanwhile, the team estimates about 143 cases of ischemic stroke for the Pfizer-BioNTech vaccine.
On the other hand, SARS-CoV-2 infection may cause an estimated 934 extra cases of thrombocytopenia, 12,614 cases of venous thromboembolism, 1,699 cases of ischemic stroke, and 20 of CVST. Thus, the risk of these vascular events is significantly higher as compared to those that might occur post-vaccination.
“The incidence rate ratios associated with SARS-CoV-2 infection were much higher for each outcome than those associated with either vaccine, with the greatest risk for all outcomes being in the first week after a positive test.”
- Hippisley, J., Patone, M., Mei, X., Saatci, D. et al. (2021). Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. British Medical Journal (BMJ) 374. doi:10.1136/bmj.n1931. https://www.bmj.com/content/374/bmj.n193
Posted in: Medical Science News | Medical Research News | Medical Condition News | Disease/Infection News | Healthcare News
Tags: Blood, Brain, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Hospital, Immunization, Ischemic Stroke, Mortality, Platelet, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stroke, Syndrome, Thrombocytopenia, Thromboembolism, Thrombosis, Vaccine, Vascular, Venous Thromboembolism

Written by
Angela Betsaida B. Laguipo
Angela is a nurse by profession and a writer by heart. She graduated with honors (Cum Laude) for her Bachelor of Nursing degree at the University of Baguio, Philippines. She is currently completing her Master's Degree where she specialized in Maternal and Child Nursing and worked as a clinical instructor and educator in the School of Nursing at the University of Baguio.
Source: Read Full Article



