Home » Health News »
E406W mutation on SARS-CoV-2 RBD escapes monoclonal antibody cocktail-mediated neutralization
The receptor-binding domain (RBD) of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike glycoprotein binds to the angiotensin-converting enzyme 2 (ACE2) receptor and initiates viral entry into cells. The SARS-CoV-2 RBD is the main therapeutic target for all neutralizing antibodies elicited by SARS-CoV-2 infection, coronavirus disease 2019 (COVID-19) vaccination, as well as monoclonal antibodies (mAbs).
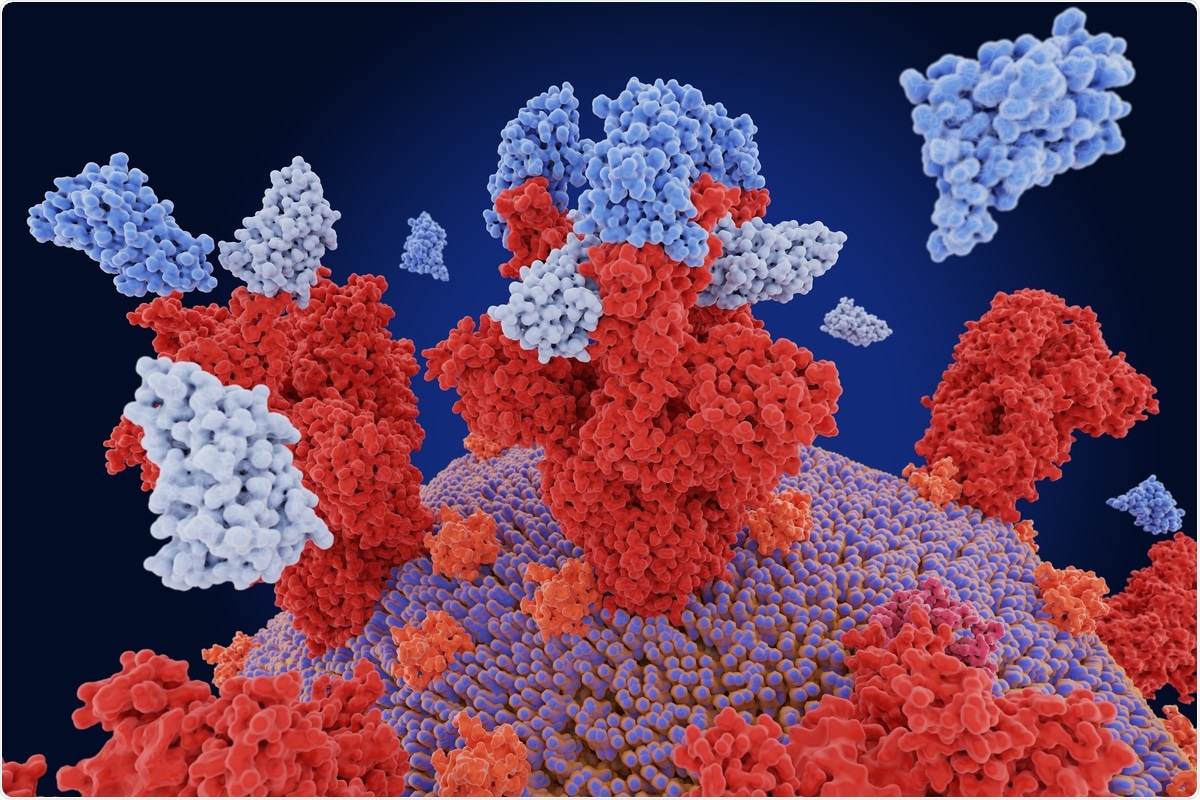 Study: Structural changes in the SARS-CoV-2 spike E406W mutant escaping a clinical monoclonal antibody cocktail. Image Credit: Juan Gaertner / Shutterstock.com
Study: Structural changes in the SARS-CoV-2 spike E406W mutant escaping a clinical monoclonal antibody cocktail. Image Credit: Juan Gaertner / Shutterstock.com
Background
A single RBD residue mutation can help the virus evade the host immune mechanism. As a result, therapeutic cocktails comprising two mAbs were formulated to recognize non-overlapping epitopes. These cocktails have at least two distinct amino-acid substitutions that make it difficult for the virus to escape neutralization.
The REGEN-COV is a type of antibody cocktail that consists of two mAbs casirivimab (REGN10933) and imdevimab (REGN10987) that bind non-overlapping RBD epitopes in the receptor-binding motif (RBM) and block ACE2 attachment for the virus. All possible RBD residue mutations that permit escape from the REGEN-COV mAb cocktail and the cilgavimab (AZD1061) mAb have been previously mapped, which helped researchers identify an E406W substitution that overrode binding and neutralization by both REGEN-COV mAbs and cilgavimab.
Residue E406 is located outside of the epitopes recognized by casirivamab, imdevimab, and cilgavimab. This observation suggests that this mutation might influence the overall structure of the RBD by retaining detectable binding to dimeric human ACE2 and preventing neutralization by antibodies.
In a recent study published on the preprint server bioRxiv*, researchers conduct a series of experiments to better understand the molecular basis of E406W-mediated escape from the REGEN-COV cocktail and cilgavimab. To this end, the researchers characterized the SARS-CoV-2 spike ectodomain trimer structure housing the E406W mutation.
About the study
The characterization process involved the three-dimensional (3D) classification of the SARS-CoV-2 spike ectodomain trimer dataset, which revealed the presence of two conformational states. Whereas one conformational state included three closed RBDs, the other included one open RBD. These structures accounted for approximately 70% and 30% of particles, respectively.
The researchers also used symmetry expansion, focused classification, and local refinement for the RBD reconstruction at 3.4Å resolution for model building and analysis.
Study findings
The researchers observed that imdevimab (REGN10987) recognized an epitope at the interface between antigenic sites Ia and IIa5 and formed extensive interactions with residues 440-449 that would sterically clash with the E406W RBD mAb heavy chain. Casirivamab (REGN10933), on the other hand, interacted with residues 417, 453-456, and 475-490 within antigenic site Ia5.
The distinct conformation of the 475-490 residues in the REGEN-COV-bound RBD and E406W apo spike structures likely precluded the mAb binding through a steric clash with the casirivamab light chain. Further, the E406W mutation disrupted the antigenic sites recognized by casirivamab (REGN10933) and imdevimab (REGN10987) allosterically, which were positioned 5 and 20Å away, respectively. Similar to imdevimab, cilgavimab (AZD1061) fails to bind to the E406W RBD due to the structural reorganization of residues 443-450 that are recognized by this mAb.
Several recently described broadly neutralizing sarbecovirus human mAbs have been found to be resilient to the observed SARS-CoV-2 antigenic drift in animal studies and capable of recognizing distinct RBD antigenic sites. The researchers examined the effect of the E406W mutation on the SARS-CoV-2 RBD on the concentration-dependent inhibition of S309, S2E12, and S2X259 against vesicular stomatitis virus (VSV) particles pseudotyped with the G614 spike or the W406/G614 spike.
Each of these three mAbs neutralized G614 and W406/G614 pseudoviruses with comparable potency, thereby indicating their efficacy against this mutant. However, the S2H14 mAb failed to neutralize the spike W406/G614 pseudovirus due to the reorganization of the RBM. These data further demonstrate that binding to the SARS-CoV-2 W406 RBD was unaffected for S2E12 and abrogated for S2H14
The researchers also assessed the impact of the E406W mutation on vaccine-elicited plasma neutralizing activity using samples obtained from individuals who had received two doses of either Pfizer BNT162b2 or Moderna mRNA-1273 COVID-19 vaccine.
To this end, there was a 2.5-fold and 2.4-fold reduction in neutralization potencies against the W406/G614 spike pseudovirus for BNT162b2 and mRNA-1273 recipients, respectively, as compared to G614 spike-harboring pseudovirus. These data indicated that the single E406W mutation led to a moderate erosion of vaccine-elicited polyclonal neutralizing antibodies that were comparable to the vaccine-evading properties of SARS-CoV-2 Epsilon or Delta variant.
Implications
The current study showed that although the E406W mutation promoted escape from REGEN-COV cocktail- and cilgavimab (AZD1061)-mediated neutralization, it required multiple nucleotide substitutions from the SARs-CoV-2 wild-type spike sequence.
Several broadly neutralizing sarbecovirus mAbs were unaffected by the E406W mutation, whereas COVID-19 messenger ribonucleic acid (mRNA) vaccine-elicited polyclonal antibodies retained a substantial fraction of their activity against this mutant.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Addetia, A., Park, Y., Starr, T., et al. (2022) Structural changes in the SARS-CoV-2 spike E406W mutant escaping a clinical monoclonal antibody cocktail. bioRxiv. doi:10.1101/2022.01.21.477288. https://www.biorxiv.org/content/10.1101/2022.01.21.477288v1.
Posted in: Medical Science News | Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Coronavirus, Coronavirus Disease COVID-19, covid-19, Efficacy, Enzyme, Glycoprotein, Monoclonal Antibody, Mutation, Nucleotide, Pseudovirus, Receptor, Respiratory, Ribonucleic Acid, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stomatitis, Syndrome, Vaccine, Virus

Written by
Sreetama Dutt
Sreetama Dutt has completed her B.Tech. in Biotechnology from SRM University in Chennai, India and holds an M.Sc. in Medical Microbiology from the University of Manchester, UK. Initially decided upon building her career in laboratory-based research, medical writing and communications happened to catch her when she least expected it. Of course, nothing is a coincidence.
Source: Read Full Article



