Home » Health News »
Engineers and surgeons develop hydrogel patch for treating collapsed airways in newborns
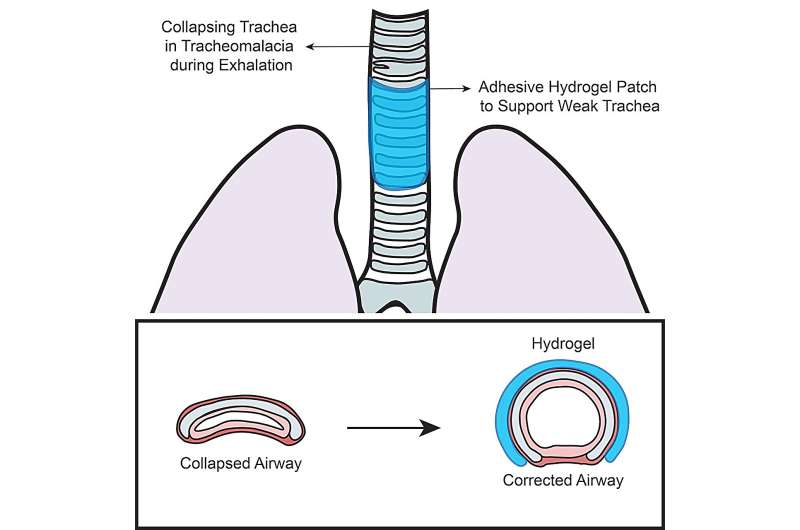
Researchers at the EPFL have achieved a breakthrough in the treatment of tracheomalacia, a condition characterized by weak tracheal cartilage and muscles that normally keep the airway open for proper breathing.
The team, composed of EPFL engineers and CHUV pediatric airway surgeons, has successfully developed a novel adhesive hydrogel patch that can effectively alleviate tracheomalacia, providing hope for improved treatment options for this challenging condition. The proof of concept was recently published in iScience.
Tracheomalacia is a relatively frequent congenital condition that often results in excessive collapse of the airway in newborns and infants. Current treatment methods such as tracheal reconstruction, tracheoplasty, and stenting often result in extensive, long-lasting damage to this vital organ. To address these limitations, the researchers and surgeons focused on developing a new strategy: to wrap a non-invasive adhesive hydrogel patch around the damaged trachea to open the airway.
Hydrogel is a biocompatible and biodegradable soft material that is increasingly being used in biomedical applications, but this is the first time bioengineers have explored its structural properties for alleviating tracheomalacia.
Using numerical and animal models, engineers Ece Uslu and Dr. Vijay Kumar Rana from the Laboratory of Biomechanical Orthopedics (LBO), have demonstrated that a hydrogel patch with suitable mechanical properties and adhesion strength could effectively maintain the physiological shape of the trachea.
To achieve this, new hydrogels are being synthesized to meet the challenging demands posed by a collapsed airway. The researchers collaborated with the Laboratory of Hemodynamics and Cardiovascular Technology (LHTC), where Sokratis Anagnostopoulos conducted crucial numerical studies.
Hydrogel patch supports collapsed airway by 50%
“This research represents a significant step forward in addressing the challenges associated with tracheomalacia treatment,” says Professor Dominique P. Pioletti, head of LBO, and lead researcher on the project. “The adhesive hydrogel patch we have developed in collaboration with the CHUV shows great promise in providing mechanical support to the trachea and preventing airway collapse.”
In this successful proof of concept, the new adhesive hydrogel patch exhibited robust adhesion on wet tracheal surfaces and structurally supported a completely collapsed trachea under negative pressure, increasing volume up to 50%. These promising results pave the way for the potential use of adhesive hydrogels as a new approach in the clinical treatment of tracheomalacia.
“We are optimistic about this proof of concept, as the 50% increase in the opening of a completely collapsed trachea is enough to alleviate the severe symptoms of tracheomalacia,” says paper co-author and CHUV pediatric surgeon Dr. Kishore Sandu.
Collaboration between EPFL engineers and CHUV pediatric surgeons
“It has been really exciting to bring together different visions and to progress towards a highly desired solution to a difficult medical problem,” says co-author of the paper and CHUV pediatric airway surgeon Dr. François Gorostidi. The fruitful collaboration between surgeons and engineers for this project depended on each side listening carefully to each other’s specific requirements in the operating room and in the lab.
“Engineers and surgeons do not always speak the same language, so we had to first understand how to work together. But coming up with an engineering solution to a medical condition with limited treatment options has proven very promising,” says Dr. Sandu.
The collaboration is ongoing, and the researchers were eager to point out that the process is extremely iterative. It’s taken three years and hundreds of formulations of the hydrogel to achieve these impressive results. And neither the surgeons or the engineers will rest until their solution to tracheomalacia reaches the operating room, solving an often-intractable problem for pediatricians who need to open the airway of newborns but risk the unavoidable and unwanted negative consequences of invasive solutions.
More information:
Ece Uslu et al, Wet adhesive hydrogels to correct malacic trachea (tracheomalacia) A proof of concept, iScience (2023). DOI: 10.1016/j.isci.2023.107168
Journal information:
iScience
Source: Read Full Article


