Home » Health News »
Multidisciplinary care improves outcomes for patients with chronic kidney disease
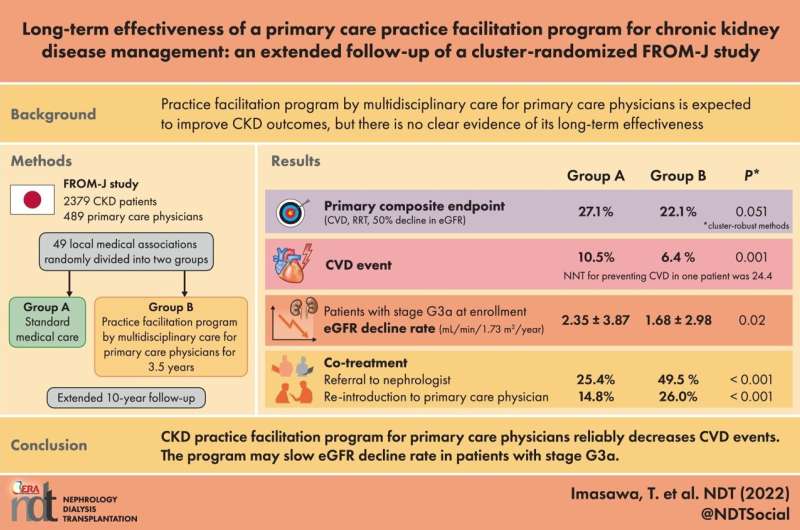
It is generally agreed that a team of individuals with unique talents and skills offers the potential to achieve more than any person can achieve alone. The Frontier of Renal Outcome Modifications in Japan (FROM-J) study, conducted from 2008 to 2012, was developed to demonstrate just that. This 3½ year study showed that intensive, multidisciplinary care that promotes direct cooperation between general practitioners (GP) and specialists improves outcomes from chronic kidney disease (CKD).
Not only is CKD a risk factor for end-stage kidney disease but it is also linked to both stroke and heart diseases, and overall health. The study’s senior author, Professor Kunihiro Yamagata, compared one group of 1,195 patients who received CKD treatment alone with a second group of 1,184 patients who received treatment along with regular interactions with a dietician, reports about their treatment responsiveness, and appointment reminders. GPs from this group received information about patients who met the criteria for referral to a nephrologist or did not visit hospitals as scheduled.
The involvement of a clinical team in patient care greatly improved treatment adherence as well as communication between GPs and nephrologists. Most importantly, this approach helped to slow the progression of CKD and led to better patient outcomes.
In a study published this month in Nephrology Dialysis Transplantation, Professor Yamagata shows the results of a 10-year follow-up of the FROM-J study. “Even seven years after the conclusion of the original study, patients in the intervention group had better kidney function and a lower rate of stroke and heart diseases than those who received CKD treatment alone,” Professor Yamagata explains.
This finding indicates that multidisciplinary care has a lasting impact on CKD patient outcomes. It is difficult to parse out which aspects of the intervention were most influential. When asked about this Professor Yamagata said, “It was likely the combined effect of multiple factors. The team not only helped to engage patients in their own care but also empowered their GPs to become more knowledgeable about what is needed to maintain the kidney, brain and heart health of CKD patients and more intense cooperation between GP and specialists were observed.”
Source: Read Full Article


