Home » Health News »
New cataract surgery options can restore your vision
Cataracts, any ophthalmologist will tell you, are an extremely common side effect of growing older. Live long enough, and most people will develop this condition—a clouding of the normally clear eye lens—in one or both of their eyes.
“As long as there have been humans, there have been cataracts,” says Vicente Diaz, MD, MBA, a Yale Medicine ophthalmologist. “For thousands of years, the goal was to get the cataract out without blinding the person. Literally, that was the goal.”
Fortunately, cataract surgery has come a long way. It is very safe, and thanks to advances in the field, patients now have many options, including laser-assisted surgery and a growing array of synthetic replacement lenses that also fix other vision problems.
“What’s great about cataract surgery now is that we not only remove the cataract, but we can restore patients’ vision,” says Yvonne Wang, MD, a Yale Medicine ophthalmologist. “They may have been wearing prescription contacts or glasses for many years. We can now put a prescription inside their new lens and give them better vision than they ever had before.”
With so many choices available, deciding what type of surgery or lens works for you might feel intimidating. We sat down with Yale Medicine cataract surgeons to answer common questions.
Cataracts defined
First, it helps to understand what a cataract is and what causes it.
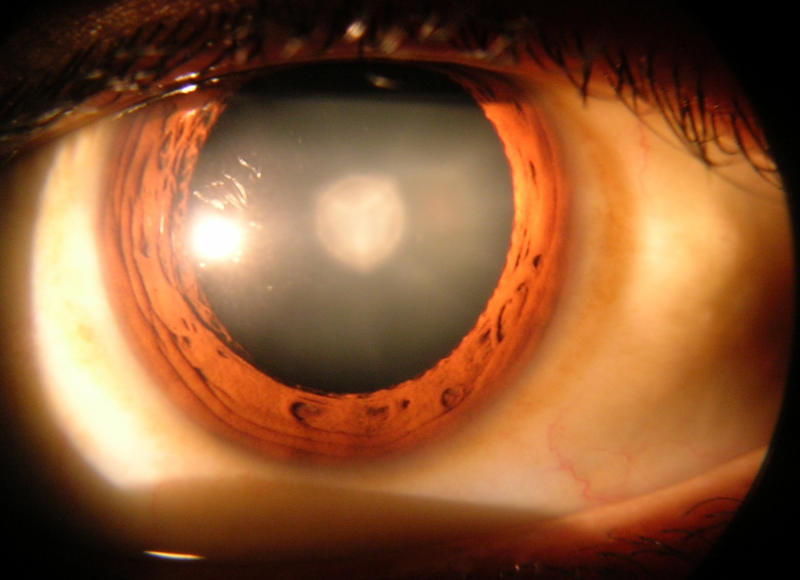
We’ll start with the lens, a structure inside of your eye that focuses light onto the retina to provide a clear image. When the lens starts to get cloudy, it blocks the light from passing through. “That’s when we call it a cataract. When one is forming, the proteins in your lenses are starting to degrade. They change in consistency and you’re no longer able to maintain clarity,” says Dr. Wang.
Blurry vision and needing to change your glasses or contacts prescription frequently are typically the earliest signs, she adds. Other symptoms can include seeing halos, as well as glare and sensitivity around lights, especially while driving at night. Or you might have trouble reading a menu in a restaurant that is dimly lit, adds Dr. Wang.
Age is the most common cause for a cataract. “It can happen at different ages. Some patients will experience it in their 50s. But the most common age for cataract surgery would be for someone in their 70s,” she says.
“In addition to age, light and UV exposure can cause the lens to become cloudy,” Dr. Wang says. “Other risk factors for cataracts can be trauma, certain medications, including steroids, certain diseases such as diabetes, and also, in rare conditions, you can be born with a cataract.”
How are cataracts diagnosed?
Ophthalmologists diagnose cataracts during an eye exam.
“I dilate the patient’s eyes and examine them through a microscope. The cataract will appear a little yellow, milky, or cloudy,” Dr. Wang says.
When a cataract is just beginning to develop and is not very large, most patients can improve their vision with an update to their glasses or contacts prescription.
“However, because cataracts worsen over time, patients may find their prescription needs to change every year or even more quickly than that—or the prescription doesn’t correct it sufficiently,” Dr. Wang says. “At that point, the only treatment is cataract surgery.”
What are my options for cataract surgery?
Once you decide to have cataract surgery, talk to your ophthalmologist about what surgical technologies are available and what kind of intraocular lens (IOL)—a synesthetic lens—you would like to use to replace the cataract.
The two types of surgery are:
- Basic cataract surgery: This is one of the most common types of surgery in the world. It involves making a small incision in the eye, breaking up the cataract with ultrasound, and removing those pieces. The surgeon then places an IOL into the lens capsule. (More on what to expect during surgery below.)
- Laser surgery: At Yale, surgeons also offer cataract surgery with a femtosecond laser, which uses high-energy, focused light beams with pulses so quick they are measured in “femtoseconds,” or trillionths of a second. The laser can make incisions and soften the cataract so that it is easier to remove. Using a laser allows for precise incisions in less time, and it may provide more fine-tuned vision correction than traditional surgery.
Laser surgery may be recommended for people who choose a specific type of IOL, such as multifocal or extended depth of focus lens (explained below). During surgery, the laser can also correct astigmatism (a condition in which the front surface of the lens is curved differently, leading to blurry vision).
What are my lens choices?
All IOLs will provide clear vision. Once you have your cataracts removed, you can keep the same vision you had before surgery (meaning if you were nearsighted before surgery, you can choose a lens that will keep you nearsighted after surgery), or you can elect to have your vision corrected by choosing an IOL that improves how well you see up close, far away, or in between. In other words, the IOL comes with a prescription, much like contact lenses or a pair of glasses.
Here are some details:
Monofocal lenses: These are the most common type of lenses used with cataract surgery. You can choose one “focusing” distance—up close, medium range, or distance vision. Most people choose to have them prescribed for distance and continue to use reading glasses to sharpen up-close vision.
You can also choose something called “monovision,” in which the lens of one eye is set to see “far” and the other one is set to see “near.” With monovision, however, because you’re using one eye for distance and one for objects up close, your binocular vision may not be as good. It’s also possible that you may lose some depth perception (the ability to judge how far away an object is). For “distance” activities, such as driving, watching TV, or going to a show or a sporting event, some people will need to wear glasses if they want both eyes to see the “distance” event.
Monovision isn’t for everyone, says Brian DeBroff, MD, a Yale Medicine ophthalmologist. “Usually, we offer it to people who have already tried it with contacts because they know what it’s like,” he says.
Multifocal lenses: These actually have corrective zones built into the lenses, similar to bifocal or trifocal glasses. Multifocal lenses allow you to see near and far objects, and some also correct intermediate vision. While multifocal lenses may enable you to ditch glasses or contacts entirely for any activity, they are associated with reports of visual disturbances, including halos and glare.
Extended depth of focus (EDOF): These lenses have only one corrective zone, but it is stretched to a single, elongated focal point. This allows for distance and intermediate vision. EDOF lenses are associated with less visual disturbances than multifocal lenses, but you may still need glasses for “near” vision.
Toric IOLs: These lenses have built-in correction for astigmatism and are available in a range of strengths, depending on your needs. They can be used across the monofocal, multifocal, and EDOF platforms. The ability to correct astigmatism during cataract surgery is exciting, Dr. Diaz says. “We can use either the laser or an intraocular lens—or a combination of both—to achieve fine-tuned results,” he says. Dr. DeBroff agrees. “This is important because multifocal lenses won’t work well if there’s an existing astigmatism,” he says.
It’s important to note that certain options, including multifocal, EDOF, and toric lenses, as well as laser surgery, may not be covered by your insurance plan.
What is the ORA system?
One of the newest advancements in cataract surgery includes a technology called ORA (Optiwave Refractive Analysis), which is a kind of intraoperative aberrometry—a tool surgeons can use to take refractive measurements in the operating room, with the goal of providing optimal lens power and placement.
“This machine takes an extra measurement of your eye during cataract surgery, which allows for a more accurate measurement of the lens that’s being placed inside it,” Dr. Wang says. “Having an accurate measurement is really important to getting the best visual outcome. The newest lens designs allow for good vision at a distance, as well as reading. But to get those good outcomes, you need to have very accurate measurements.”
Traditionally, when someone is preparing to have cataract surgery, surgeons take measurements of the size and shape of their eye so they can predict what lens they need, Dr. Diaz explains. “But cataracts can throw off that measurement. ORA allows us to measure the eye again once we remove the cataract, and this tends to be more accurate, leading to a more accurate lens placement and, therefore, better vision,” he says.
What is cataract surgery like?
Cataract surgery is a common, safe procedure, Dr. Wang says. It is performed in an outpatient setting with patients returning home the same day. Patients have surgery done in one eye and typically return for the second eye after a few weeks.
“The whole experience of cataract surgery only takes a few hours, but the surgery itself only takes 15 to 20 minutes on an average case,” Dr. Wang says.
First, your eye is numbed with a local anesthetic (either eye drops or an injection). You remain awake during the procedure, but you are given light sedation through an IV to make you relaxed and comfortable, Dr. Wang explains.
“The surgery is overall fairly painless,” she says. “Most patients will complain of a little itching or irritation overnight during the first night. And their vision typically improves by the next day.”
Patients will go home with a shield over their eye for the first day and then wear it only at night for one week.
“We recommend patients just take it easy and only do light activity—no heavy lifting or bending,” says Dr. Wang. “Other than that, you can usually go back to work within a day or two.”
Source: Read Full Article


