Home » Health News »
Researchers collaborate on universal antibody test for COVID-19
Researchers with the U.S. Army Futures Command are part of a team that tested alternative ways to measure COVID-19 antibody levels, resulting in a process that is faster, easier and less expensive to use on a large scale. Their method holds promise for accurately identifying potential donors who have the best chance of helping infected patients through convalescent plasma therapy.
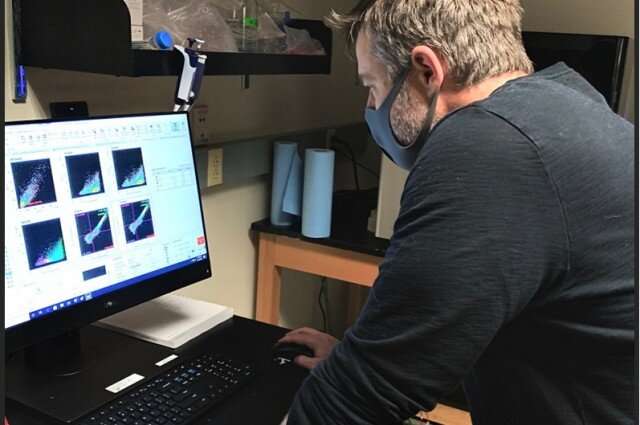
Dr. Jimmy Gollihar, biochemist and biotechnologist for the U.S. Army Combat Capabilities Development Command’s Army Research Laboratory at CCDC ARL South in Austin, Texas, and chief technology officer of the Bioindustrial Manufacturing Innovation Institute, in collaboration with Dr. John Dye at the U.S. Army Medical Research Institute of Infectious Diseases, or USAMRIID, and collaborators at Houston Methodist, Pennsylvania State University and the University of Texas at Austin, sought to find alternatives to measuring virus neutralization, or VN, titers. These titers are the gold standard of COVID-19 antibody testing, as VN antibodies in the blood have been shown to correlate with levels of protective immunity.
According to the researchers, this kind of antibody testing is not widely available as it is technically complex and requires days to set up, run and interpret. Thus, the team looked to another type of test, called enzyme-linked immunosorbent assays, or ELISAs.
According to Gollihar, ELISAs are standard quantitative tests used to measure the amount of antibody to a particular antigen in a given sample.
“ELISAs are standard assays that can be performed in almost any academic or medical laboratory,” Gollihar said. “This is important in emergency care centers treating critically ill patients. The assays can also be used for serological monitoring of the disease.”
Specifically, scientists looked at the relationship of anti-spike ectodomain, or ECD, and anti-receptor binding domain, or RBD, antibody titers in the bloodstream. The spike ECD and RBD proteins are components of the much-talked-about spike protein made by SARS-CoV-2 and are critical to how the virus enters the body, spreads and causes COVID-19 disease.
Gollihar’s specific roles included coordinating the plasma sample delivery from Houston Methodist, scaling production and purification of the antigens, and setting up the collaboration with USAMRIID for live virus neutralization testing under biocontainment conditions. He also helped transition the ELISA assay to Houston Methodist’s automation team.Dye and his team performed neutralization assays on all the specimens in a Biosafety Level 3 laboratory at USAMRIID.
Their work determined that the relative amount of antibody in the bloodstream of COVID-19 patients is linked to their ability to control viral infection; essentially, the more severe the disease, the higher the levels of neutralizing antibody present. This information provides potential benchmarks for a clinical product for convalescent plasma treatment studies; it could also be used to assess how well a vaccine recipient may respond to a subsequent infection.
The researchers found that the ELISA tests had an 80 percent or greater probability of predicting VN titers at or above the Food and Drug Administration-recommended levels for COVID-19 convalescent plasma.
“In all, we discovered that high titer ELISAs correlate well to virus neutralization and can be used as a surrogate for screening convalescent plasma,” Gollihar said.
In addition, the researchers found that convalescent donors maintain high levels of immunity over the course of many weeks, and that frequent plasma donations did not cause a significant decrease in antibody or virus neutralization levels.
Perhaps most surprising, the researchers said, is that they identified 27 individuals from the surveillance cohort with high enough antibody titers to indicate that some asymptomatic individuals may have plasma suitable for therapeutic use and may have a degree of relative immunity against SARS-CoV-2.
“This collaboration between the Army, Houston Methodist and our partners in academia shows the incredible diversity of complementary capabilities we can deploy in responding to a worldwide pandemic,” Dye said.
Source: Read Full Article


