Home » Health News »
Researchers identify a potent new combination of antiviral drugs to combat SARS-CoV-2
Coronavirus disease 2019 (COVID-19) overwhelmed healthcare services worldwide when it first emerged, and the lack of immediate treatment frustrated healthcare workers. Instead of treating the infection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), they were forced to treat the symptoms using supplemental oxygen and invasive mechanical ventilation. The recent success of Paxlovid has encouraged researchers to develop new anti-covid drugs. With this in mind, scientists from the University of Pennsylvania have been investigating a new synergistic treatment. Their research is released early as an unedited version of the manuscript to be published in the journal Nature.
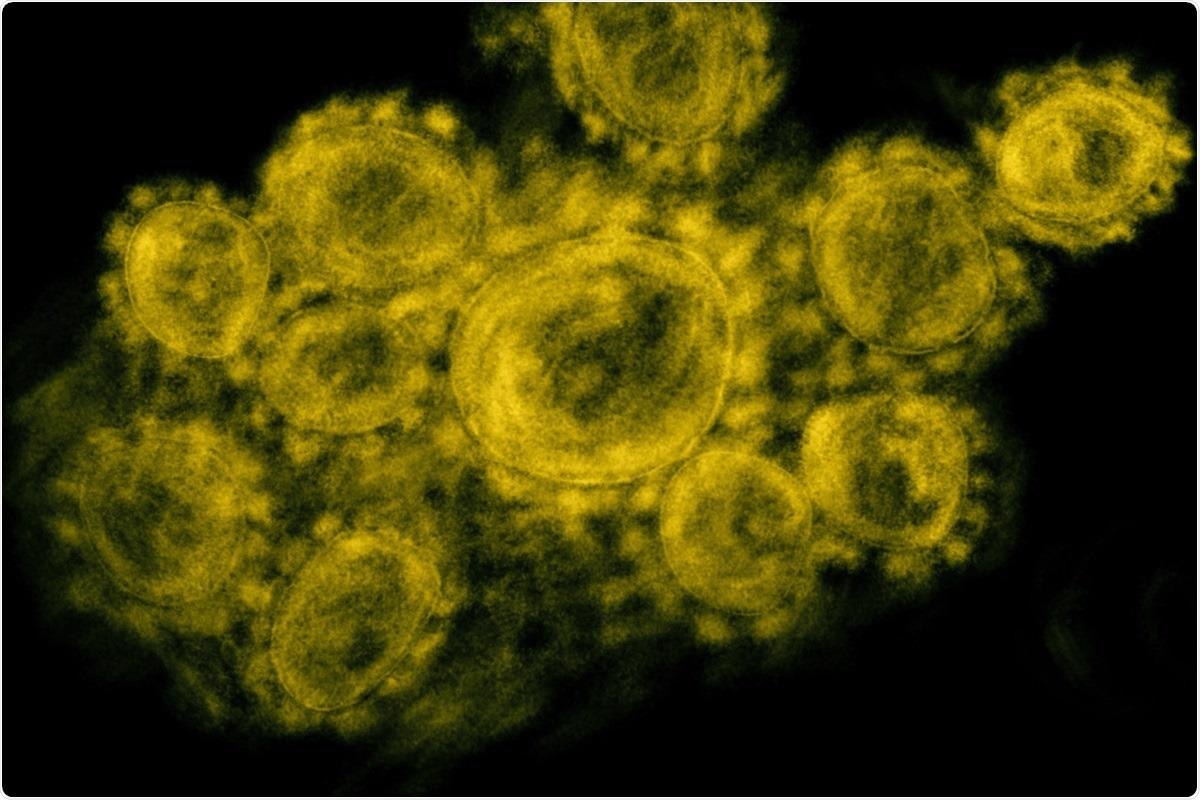
Study: Pyrimidine inhibitors synergize with nucleoside analogues to block SARS-CoV-2. Image Credit: Pong Ch / Shutterstock
The Study
The researchers managed to screen ~18,000 drugs from three different repurposing libraries. Most of the candidates came from the ReFrame collection (around 11,300), while the rest came from their in-house library (PENN library) and the NCATS repurposing collection.
The PENN library revealed 77 drugs that could potentially inhibit SARS-CoV-2 infection, the NCATS library 45, and the ReFrame collection 135. Following validation, 122 compounds remained. 13% of these were nucleoside analogs, a common class of drugs that can be incorporated by polymerases into DNA/RNA, inhibiting cell division. They can act as antimetabolites by competing with enzymes for natural ligands – typically used to treat cancer/autoimmune diseases, and a small subset can act as direct antivirals. This subset is explicitly incorporated by viral polymerases. Two of these direct antivirals have already shown significant ability to combat SARS-CoV-2 and have been approved for use in humans – remdesivir and molnupiravir. Both of these were identified in the screening panels alongside 13 additional antiviral nucleoside analogs.
To test the ability of the identified compounds, the researchers tested a panel of cell lines known to be permissive to SARS-CoV-2 infection, including hACE2 expressing A549, Caco-2, Huh7.5, and Vero cells.
As expected, remdesivir and molnupiravir showed significant ability across all cell types – which was further validated in Calu-3 cells using quantitative RT-qPCR assays. The antivirals that worked by competing for natural ligands were found to be non-toxic at the concentrations used, but showed differing antiviral activity in different cell types.
Tubercidin showed antiviral activity in Calu-3, Caco-2 and Huh7.5 cells but was toxic in A549-Ace2 and Vero cells, while thioguanine and 6-Mercaptopurine were active in Calu-3 and A549-Ace2 cells but not Caco-2 or Vero cells.
When performing the same RT-qPCR assays as used for remdesivir and molnupiravir, all nucleoside analogs showed significant antiviral activity, but when a subset of the antiviral nucleosides was tested in primary human nasal air-liquid interface cultures, only remdesivir and molnupiravir showed any significant antiviral activity.
The researchers then examined the possibility of synergy between remdesivir and molnupiravir, as they were curious about the possibility that if the two drugs were applied together, they could have more than an additive effect. They treated Calu-3 cells with six different concentrations of each drug individually and in combination with each other, resulting in 36 different conditions. They used BLISS analysis to determine if there was any effect, with the null hypothesis that the drugs were additive. Unfortunately, this was found to be the case.
Following this, the scientists examined a subset of nucleosides that inhibited the pyrimidine and purine biosynthetic pathways. Three drugs were included in this, the DHODH inhibitors BAY-2402234 and Brequinar, and the UMPS inhibitor pyrazofurin. These drugs were found to be active in Calu-3 cells without toxicity, and the DHODH inhibitors showed activity in A549-Ace2 cells, with pyrazofurin showing slightly less effect. Both the DHODH inhibitors also showed significant synergy with both Molnupiravir and remdesivir.
As different SARS-CoV-2 variants have continued to emerge with devastating effects, the researchers followed this by investigating the ability of these drugs to counter different variants. Molnupiravir, remdesivir, and the pyrimidine biosynthesis inhibitor were all effective against all variants.
After further testing, the researchers moved to a mouse model, testing the approved Molnupiravir and Brequinar, individually and in combination. As expected, molnupiravir showed a dose-dependent reduction in viral titer. Brequinar had no effect alone, but a combined treatment resulted in a -4 log reduction in viral titers, strong suppression of lung inflammation, and protection of lung architecture even at low doses.
The Conclusion
The authors have successfully shown that a combination of nucleoside analogs and DHODH inhibitors are powerful anti-COVID agents in mice models and strongly suggest that this treatment be explored further in clinical trials. While many western countries have controlled the pandemic through mass-vaccination schemes, the developing world is still struggling with the pandemic, and new variants continue to threaten the ability to push through vaccine protections, so this study provides welcome news for new drugs that could help end the pandemic.
- Schultz, D.C., Johnson, R.M., Ayyanathan, K. et al. Pyrimidine inhibitors synergize with nucleoside analogues to block SARS-CoV-2. Nature (2022). https://doi.org/10.1038/s41586-022-04482-x, https://www.nature.com/articles/s41586-022-04482-x
Posted in: Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: ACE2, Cancer, Cell, Cell Division, Coronavirus, Coronavirus Disease COVID-19, covid-19, DNA, Drugs, Healthcare, Inflammation, Mouse Model, Nucleoside, Oxygen, Pandemic, Purine, Pyrimidine, Remdesivir, Research, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Vaccine

Written by
Sam Hancock
Sam completed his MSci in Genetics at the University of Nottingham in 2019, fuelled initially by an interest in genetic ageing. As part of his degree, he also investigated the role of rnh genes in originless replication in archaea.
Source: Read Full Article



