Home » Health News »
Wastewater monitoring took off during the COVID-19 pandemic: How it could help head off future outbreaks

A community’s sewage holds clues about its COVID-19 burden. Over the course of the pandemic, wastewater surveillance has become an increasingly popular way to try to understand local infection trends.
Microbiologists Susan De Long and Carol Wilusz met and became wastewater aficionados in April 2020 when a grassroots group of wastewater treatment plant operators asked them to develop and deploy a test to detect SARS-CoV-2 in samples from the sewers of Colorado. De Long is an environmental engineer who studies useful bacteria. Wilusz’s expertise is in RNA biology. Here they describe how wastewater surveillance works and what it could do in a post-pandemic future.
How is wastewater monitored for SARS-CoV-2?
Wastewater surveillance takes advantage of the fact that many human pathogens and products of human drug metabolism end up in urine, feces or both. The SARS-CoV-2 virus that causes COVID-19 shows up in surprisingly large quantities in feces of infected people, even though this is not a major route of disease transmission.
To figure out whether any pathogens are present, we first need to collect a representative sample of wastewater, either directly from the sewer or at the point where what engineers call “influent” enters a treatment plant. We can also use solids that have settled out of the wastewater.
Technicians then need to remove large particles of fecal matter and concentrate any microbes or viruses. The next step is extracting their nucleic acids—the DNA or RNA that holds the pathogens’ genetic information.
The sequences contained in the DNA or RNA act as unique bar codes for the pathogens present. For instance, if we detect genes that are unique to SARS-CoV-2, we know that the coronavirus is in our sample. We use PCR-based approaches, similar to those used in clinical diagnostic tests, to detect and quantify SARS-CoV-2 sequences.
Characterizing the nucleic acid sequence in more detail can provide information about viral strains—for instance, it can identify variants like omicron BA.2.
Currently, the vast majority of wastewater surveillance efforts are focused on SARS-CoV-2, but the same techniques work with other pathogens, including poliovirus, influenza and noroviruses.
Before the pandemic, one application was monitoring for rare poliovirus outbreaks in areas where polio vaccination is ongoing. Wastewater can also be monitored for signs of various drugs to give insights into the level and type of drug use in a population.

Where does the data go?
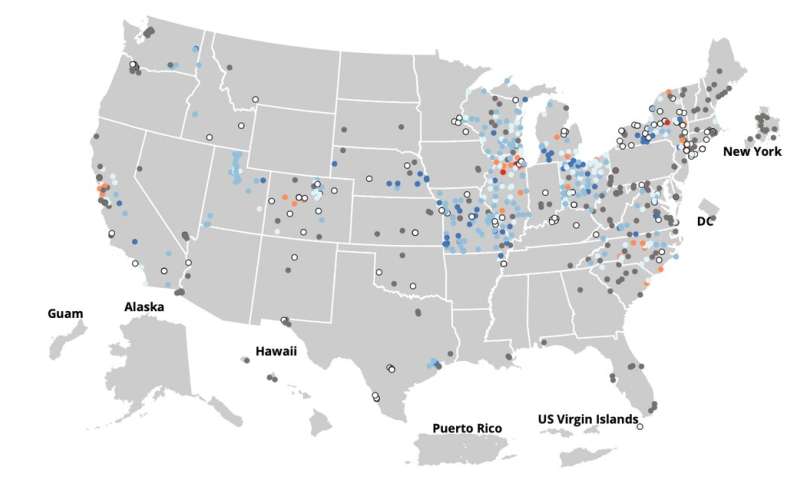
During the pandemic, the U.S. Centers for Disease Control and Prevention developed the National Wastewater Surveillance System specifically to track SARS-CoV-2 across the country. Over 800 sites report data to this NWSS system, but not all states and counties are currently represented.
Many state agencies, like the Colorado Department of Public Health and Environment, and cities, like Tempe, Arizona, have their own dashboards for reporting data. Some companies performing wastewater analysis report data on their own dashboards, too.
In our opinion, the NWSS represents an exciting first step in monitoring population health through wastewater. Similar systems are being established in other countries, including Australia and New Zealand.
What does wastewater data really show?
SARS-CoV-2 levels in wastewater from large populations are an excellent indicator of the infection level in a community. The system automatically monitors everyone who lives in the sewershed, so it’s anonymous, unbiased and equitable. Importantly, it is also impossible to track the infection back to a particular person, household or neighborhood without taking additional samples.
Wastewater surveillance doesn’t rely on the availability of clinical tests or people reporting their test results. It also picks up asymptomatic and pre-symptomatic cases of COVID-19; this is critical because people who are infected but don’t feel sick can still spread COVID-19.
In our opinion, wastewater testing is increasingly important as more COVID-19 tests are done at home. And because vaccination has also led to more mild and asymptomatic cases of COVID-19, people may be infected without getting tested at all. These factors mean that clinical case data are less informative than earlier in the pandemic, while wastewater data remains a consistent indicator of community infection level.
So far, you can’t accurately predict the number of infected individuals in a community based on the level of virus in its wastewater. The stage of someone’s infection, how their body responds to the virus, the viral variant, how far a person was from where the wastewater sample was taken, even the weather can all affect the amounts of SARS-CoV-2 measured in sewage.
But scientists can infer relative changes in infection rates. Watching viral levels go up and down in sewage provides a glimpse of whether cases are rising or falling in the community as a whole.
Because SARS-CoV-2 can be detected in wastewater days or even weeks before outbreaks occur, wastewater monitoring can provide an early warning that public health measures may be warranted. And trends in the signal are important—if you know levels are rising, it may be a good time to reinstitute a mask mandate or recommend working from home. At present, public health officials use wastewater monitoring data along with other information like test positivity rates and the number of clinical cases and hospitalizations in the community to make these kinds of decisions.
Data from sequencing can also help detect new variants and monitor their levels, allowing health responses to take into account the characteristics of the variant present.
In smaller populations, such as in college dormitories and nursing homes, wastewater monitoring can detect a small number of infected people. That can sound the alarm that targeted clinical testing is in order to identify infected people for isolation. Early detection, targeted testing and quarantining are effective at preventing outbreaks. Rather than using clinical testing for routine monitoring, administrators can reserve disruptive clinical tests for times when SARS-CoV-2 is detected in the wastewater.
What will monitoring look like in the future?
Widespread and routine use of wastewater monitoring would give public health officials access to information about the levels of a range of potential infections in U.S. communities. This data could guide decisions about where to provide additional resources to communities, like holding testing or vaccination clinics in places where infection is on the rise. It could also help determine when interventions like masking or school closures are necessary.
In the best case, wastewater monitoring might catch a new virus when it first arrives in a new area; an early shutdown in the very localized area could potentially prevent a future pandemic. Interestingly, researchers have detected SARS-CoV-2 in archived wastewater samples collected before anyone had been diagnosed with COVID-19. If wastewater monitoring had been part of the established public health infrastructure back in late 2019, it could have provided an earlier warning that SARS-CoV-2 was becoming a global threat.
For now, though, establishing and operating a national wastewater surveillance system, particularly one that includes building-level monitoring at key locations, is still too costly and labor-intensive.
Source: Read Full Article


