Home » Health News »
Women with rheumatoid arthritis more likely to achieve remission if they take sex hormones, finds research
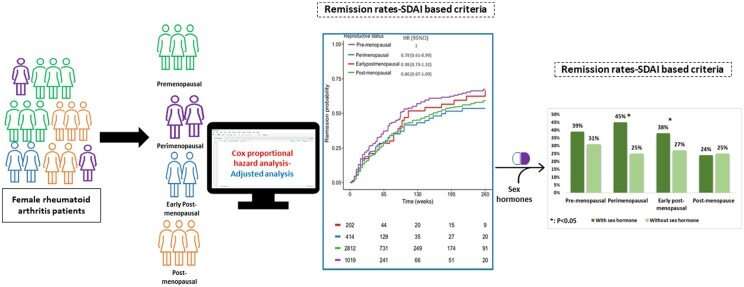
A large study of women with rheumatoid arthritis has found that those taking oral contraceptives or hormone replacement therapy (HRT) had a greater chance of achieving remission.
Led by the University of South Australia, researchers made the link between remission, reproductive status, and sex hormone use, after assessing data from 4474 female rheumatoid arthritis (RA) patients treated with the anti-inflammatory drug Tocilizumab and other immuno-suppressive medications.
The study revealed the following:
- Pre-menopausal women (those still experiencing a regular menstrual cycle) reported fewer RA symptoms than peri-menopausal (irregular or infrequent periods) or post-menopausal women with RA.
- RA patients using HRT or oral contraceptives in combination with the drugs prescribed for rheumatoid arthritis had a much greater likelihood of remission.
- Post-menopausal women, comprising 63% of the participants, of whom only 8% were using HRT, were less likely to achieve RA remission compared to pre-menopausal women.
The findings suggest that female sex hormones could play a major role in improving the outcome of women taking drugs prescribed for rheumatoid arthritis.
Remission rates were higher in some groups of women who were taking HRT or oral contraceptives at the same time they were taking medicines for RA, and in fact, RA remission was twice as high in peri-menopausal women.
Lead researcher UniSA Associate Professor Michael Wiese says it’s premature to say that HRT and oral contraceptives have a protective effect against rheumatoid arthritis, but the study has revealed a potential connection.
“We looked at whether women who used oral contraceptives or HRT had different outcomes when treated with drugs for rheumatoid arthritis. We found that women entering menopause who were not taking HRT or contraceptives were less likely to achieve remission compared with RA women still experiencing a regular menstrual cycle,” Assoc Prof Wiese says.
“The decision to use HRT is a complex one,” Assoc Prof Wiese says. “It does improve menopause symptoms, but it can modify the risk of some cancers and cardiovascular disease. This study suggests it could also be beneficial for women with rheumatoid arthritis, but the decision to use it requires an in-depth discussion with a general practitioner because each woman has different risk factors.”
Rheumatoid arthritis is an autoimmune inflammatory condition that is four times more prevalent in women aged under 50 years than men in the same age bracket and is twice as common in women over 60 years.
Compared with males, rheumatoid arthritis is more aggressive in women and the prognosis is worse.
“The peak age of onset of rheumatoid arthritis among females is 45-55 years, corresponding with a drop in estrogen when women typically enter a peri-menopausal period, where their periods become irregular.
“Furthermore, at the onset of menopause there is an increase in pro-inflammatory proteins.”
Early menopause, or menopause that occurs in women under 45 years, increases the risk of developing rheumatoid arthritis and the incidence also sharply spikes in post-menopausal women.
Conversely, younger women with rheumatoid arthritis who fall pregnant experience a 50% decline in inflammatory activity.
The study has been published in the latest issue of Rheumatology.
Early post-menopausal women (post-menopausal women aged <45 years) made up 5% of the participants, 25% were pre-menopausal (still experiencing a regular menstrual cycle), 9% were peri-menopausal, experiencing intermittent and irregular periods, and 63% post-menopausal.
Rheumatoid arthritis affects up to 2% of the population worldwide and is primarily genetic. It mainly causes joint disease but can also affect the whole body, including organs.
More information:
Dala N Daraghmeh et al, Female reproductive status and exogenous sex hormone use in rheumatoid arthritis patients treated with tocilizumab and csDMARDs, Rheumatology (2022). DOI: 10.1093/rheumatology/keac357
Journal information:
Rheumatology
Source: Read Full Article



