Home » Health News »
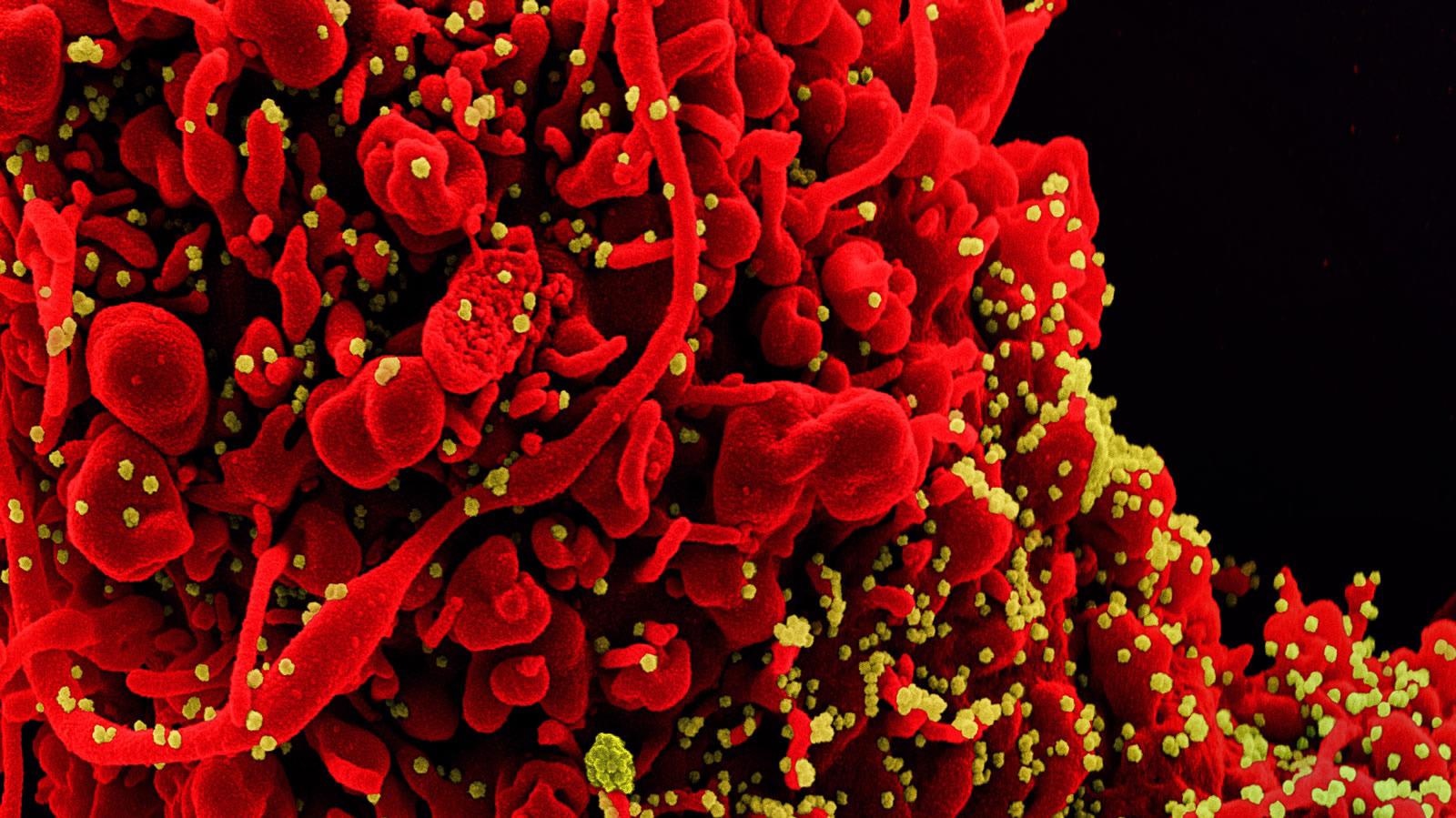
SARS-CoV-2 ORF10 degrades mitochondrial antiviral signaling protein to suppress immune response
Coronaviruses (CoVs) infect humans, pigs, cattle, horses, rats, and bats, among other host species. These viruses mainly cause infections of the respiratory and digestive tracts, with a wide range of clinical symptoms.
In humans, CoVs were once thought to be relatively harmless respiratory infections. Zoonotic CoVs, on the other hand, have crossed species boundaries, resulting in novel CoVs that can transfer from animals to humans.
For example, SARS-CoV caused SARS outbreaks in 2002 and 2003, MERS-CoV emerged in 2012 and continues to circulate in camels, and the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease 2019 (COVID-19), emerged in December 2019 and is responsible for the current severe COVID-19 outbreak worldwide, which has resulted in significant morbidity and mortality.
As a result, it is critical to have a deeper understanding of the molecular mechanisms behind viral infection and dissemination in the body.
With a length of 29.9 kb, the SARS-CoV-2 genome is a positive-sense, nonsegmented, single-stranded RNA. SARS-CoV-2 has 14 open reading frames (ORFs) flanked by 5′ and 3′ untranslated regions in its genome. ORF1a and ORF1b, which encode polyproteins that are subsequently cleaved to create 16 non-structural proteins (nsps) that make up the viral replicase-transcriptase complex, account for around two-thirds of the viral RNA genome. The spike (S), envelope (E), membrane (M), and nucleocapsid (N) proteins, which are components of the virion, are encoded by ORFs in a third of the genome around the 3′ terminus.
SARS-CoV-2 ORF10 reduces innate immunity and enhances viral replication by activating mitophagy to break down mitochondrial antiviral signaling protein (MAVS), as shown in new research out of China.
ORF10 binds to Nip3-like protein X (NIX) and microtubule-associated protein 1 light chain 3 B (LC3B), then translocates to mitochondria, inducing mitophagy and MAVS destruction. NIX is also implicated in the ORF10-mediated degradation of MAVS and the inhibition of IFN responses, according to the research.
The research is published in the journal Cellular & Molecular Immunology.
The study
SARS-CoV-2 employs a number of techniques to prevent the generation of type I interferons (IFN-I,) allowing the virus to replicate quickly and avoid host antiviral responses. HeLa- angiotensin-converting enzyme 2 (ACE2) cells were transfected with ORF10-HA and an empty vector (pCMV-HA) to investigate the role of ORF10 in the antiviral innate immune response. Whole-cell lysates were then investigated using quantitative real-time PCR (qRT–PCR) and western blotting.
When stimulated with poly(I:C) or infected with SARS-CoV-2, overexpression of ORF10 significantly reduced transcription of the IFN-1 and IFN- genes.
The researchers also discovered that overexpression of ORF10 inhibited the production of IFN- in HeLa cells when stimulated with poly(I:C) (I:C). Following that, the effect of ORF10 expression on antiviral ISGs was investigated, and it was discovered that after poly(I:C) treatment or SARS-CoV-2 infection, ORF10 expression lowered the mRNA levels of ISG15 and OAS1 relative to control cells.
Mitochondrial MAVS connects antiviral type I IFN signaling to mitochondria. Some viruses cause mitophagy, which results in mitochondrial fragmentation and, as a result, a reduction in innate immunity.
In SARS-CoV-2-infected cells, green fluorescent protein- (GFP-)tagged LC3 colocalized with DsRed-tagged Mito, a mitochondrial marker protein, showing that SARS-CoV-2 infection triggered mitophagy.
Furthermore, treatment with bafilomycin A1 (BafA1) or mitochondrial division inhibitor 1 (Mdivi-1) prevented MAVS degradation generated by SARS-CoV-2 infection, implying that SARS-CoV-2 infection causes MAVS degradation via mitophagy.
To see if ORF10 inhibits MAVS protein expression by triggering mitophagy, the authors looked at where ORF10 is found in mitochondria.
In ORF10-GFP-transfected HeLa cells, immunofluorescence analysis revealed that GFP-tagged ORF10 colocalized with DsRed-tagged Mito.
The next step was to see if ORF10 could trigger mitophagy. In ORF10-HA-transfected HeLa cells, immunofluorescence examination revealed that GFP-tagged LC3B colocalized with DsRed-tagged Mito, showing that ORF10 caused LC3 localization in mitochondria.
Furthermore, the authors detected the expression of the outer membrane mitochondrial protein TOMM20, a mitochondrial marker protein. They discovered that ORF10 expression decreased translocase of outer mitochondrial membrane 20 (TOMM20) expression, which was prevented by Baf A1 treatment. SARS-CoV-2 ORF10 destroys the MAVS protein via mitophagy, according to these findings.
Implications
The authors of this paper describe how the SARS-CoV-2 ORF10 protein suppresses innate antiviral defense and promotes viral replication. These data suggest that ORF10 interacts with NIX and LC3B to trigger mitophagy, resulting in MAVS-mediated antiviral signaling being blocked.
The findings of this work open up new avenues for research into the molecular mechanisms by which SARS-CoV-2 evades innate antiviral immunity.
- SARS-CoV-2 ORF10 suppresses the antiviral innate immune response by degrading MAVS through mitophagy, Xingyu Li, Peili Hou, Wenqing Ma, Xuefeng Wang, Hongmei Wang, Zhangping Yu, Huasong Chang, Tiecheng Wang, Song Jin, Xue Wang, Wenqi Wang, Yudong Zhao, Yong Zhao, Chunqing Xu, Xiaomei Ma, Yuwei Gao & Hongbin He, Nature, 2021.11.29, https://www.nature.com/articles/s41423-021-00807-4
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Cell, Coronavirus, Enzyme, Fluorescent Protein, Genes, Genome, HeLa Cells, Immune Response, immunity, Immunology, Interferons, Membrane, MERS-CoV, Mitochondria, Mortality, Protein, Protein Expression, Research, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Transcription, Virus
.jpg)
Written by
Colin Lightfoot
Colin graduated from the University of Chester with a B.Sc. in Biomedical Science in 2020. Since completing his undergraduate degree, he worked for NHS England as an Associate Practitioner, responsible for testing inpatients for COVID-19 on admission.
Source: Read Full Article



